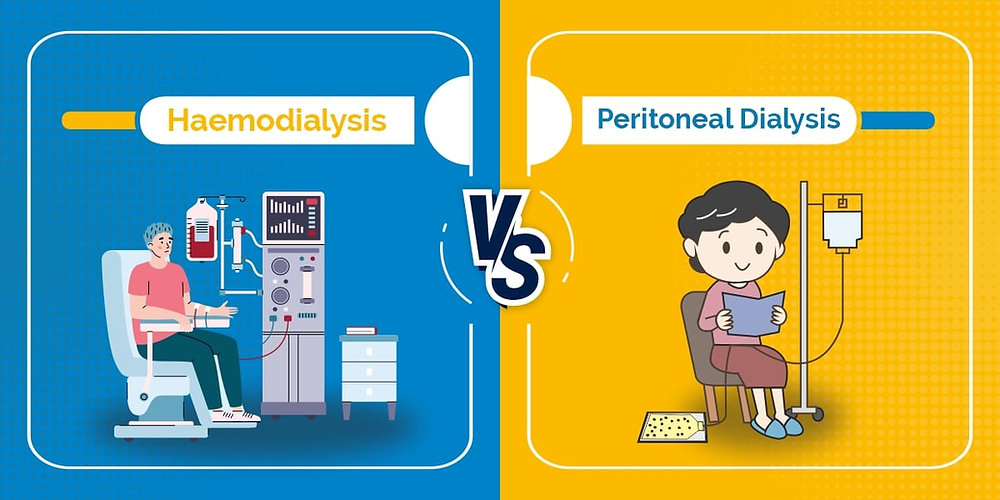
Hemodialysis Vs Peritoneal Dialysis – which modality of dialysis is better for my patient
Hemodialysis and peritoneal dialysis are two different methods of renal replacement therapy used to treat individuals with end-stage kidney disease (ESKD). Both methods have their advantages and disadvantages, and the choice between them depends on various factors including the patient’s health, lifestyle, and preferences. Here’s a comparison between hemodialysis and peritoneal dialysis:
- Method of Dialysis:
- Hemodialysis (HD): Hemodialysis is an extracorporeal process where a machine is used to filter blood outside the body. Blood is pumped through a dialyzer, a specialized filter, to remove waste products and excess fluids.
- Peritoneal Dialysis (PD): Peritoneal dialysis involves using the peritoneal membrane (a lining inside the abdomen) as a natural filter. A special solution (dialysate) is introduced into the abdominal cavity, and waste products and excess fluids pass from the bloodstream into the dialysate through the peritoneal membrane.
- 2. Location:
- Hemodialysis: Typically performed in a specialized dialysis center or hospital. Patients need to travel to the center several times a week for treatment.
- Peritoneal Dialysis: Can be done at home, which offers more flexibility and eliminates the need for frequent trips to a dialysis center. It can also be done at work or during travel, making it more convenient for some patients.
- 3. Frequency:
- Hemodialysis: Usually done 3 times a week, with each session lasting 3-5 hours. This is a more time-consuming treatment.
- Peritoneal Dialysis: Typically performed daily, and it can be done while the patient sleeps (continuous ambulatory peritoneal dialysis, or CAPD) or with the assistance of a machine (automated peritoneal dialysis, or APD).
- 4. Vascular Access:
- Hemodialysis: Requires a vascular access, usually achieved through an arteriovenous (AV) fistula, graft, or central venous catheter.
- Peritoneal Dialysis: Requires the placement of a catheter in the abdomen for infusion and drainage of dialysate.
- 5. Complications:
- Hemodialysis: Potential complications include access site infections, clotting issues, and changes in blood pressure during treatment.
- Peritoneal Dialysis: Potential complications include peritonitis (infection of the abdominal lining), catheter-related issues, and hernias.
- 6. Diet and Fluid Restriction:
- Hemodialysis: Generally requires more dietary and fluid restrictions due to the less frequent treatment schedule.
- Peritoneal Dialysis: Offers more flexibility in diet and fluid intake because it is performed daily, allowing for better toxin and fluid removal.
- 7. Quality of Life:
- Hemodialysis: May have a more structured treatment schedule and involve more time spent at a dialysis center, which can impact a patient’s daily life.
- Peritoneal Dialysis: Offers more independence and flexibility, as it can be done at home, work, or while traveling.
The choice between hemodialysis and peritoneal dialysis depends on various factors, including the patient’s health, lifestyle, and preferences, as well as medical considerations like vascular access and the presence of abdominal adhesions or infections. Nephrologists work closely with patients to determine the most suitable dialysis method for their individual needs.
Leave a Reply